Arthritis
Understanding foot arthritis and its management
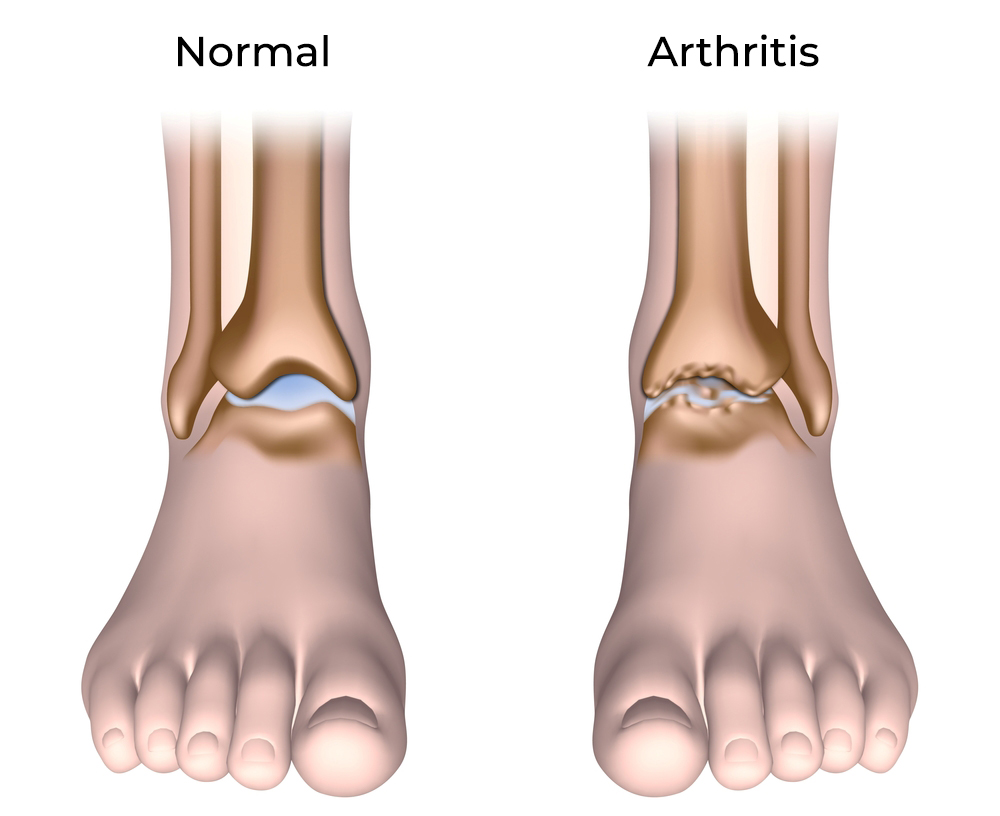
Foot arthritis is a degenerative condition that gradually wears away the cartilage in joints, leading to pain, swelling, and limited mobility. Initially, you may notice stiffness and aching in the affected joint. As the cartilage deteriorates, bones begin to rub against each other, causing discomfort and eventually leading to the formation of bone spurs. While this condition can be painful, it can be effectively managed with proper care, including the use of orthotics, footwear modifications, and in some cases, surgery.
Types of athritis
- Osteoarthritis
- Rheumatoid arthritis
- Juvenile Idiopathic arthritis
- Reactive arthritis
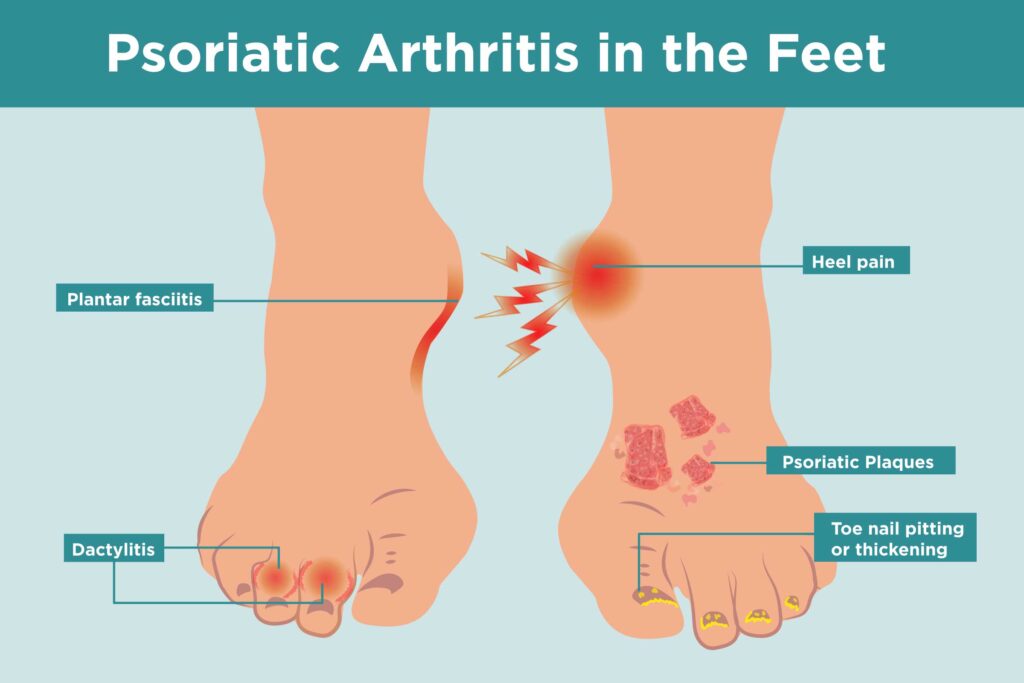
- Psoriatic arthritis
- Ankylosing Spondylitis
- Fibromyalgia
- Gout
- Lupus
- Scleroderma
- Polymyalgia Rheumatica
Joints commonly affected
Our feet endure constant stress as they support and propel our bodies, making them vulnerable to arthritis. Commonly affected areas include:
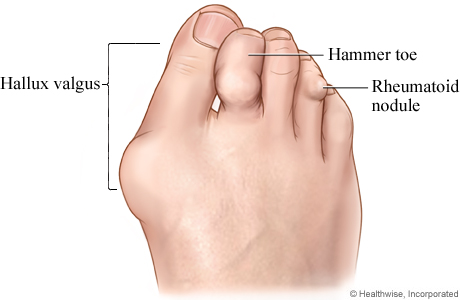
- The Big Toe Joint: Arthritis in the big toe can cause pain during movement, particularly when pushing off the ground. This condition often coexists with bunions.
- Mid-Foot and Rear-Foot Joints: Arthritis in these joints causes pain when weight is placed on the foot, often affecting the joint where the ankle and foot meet.
Diagnosing
Diagnosis typically begins with a physical exam where your medical history is reviewed, and your feet are checked for skin changes, swelling, and range of motion in affected joints. If necessary, imaging tests such as X-rays or MRIs are conducted to assess the extent of joint damage.
Types of arthritis affecting the feet
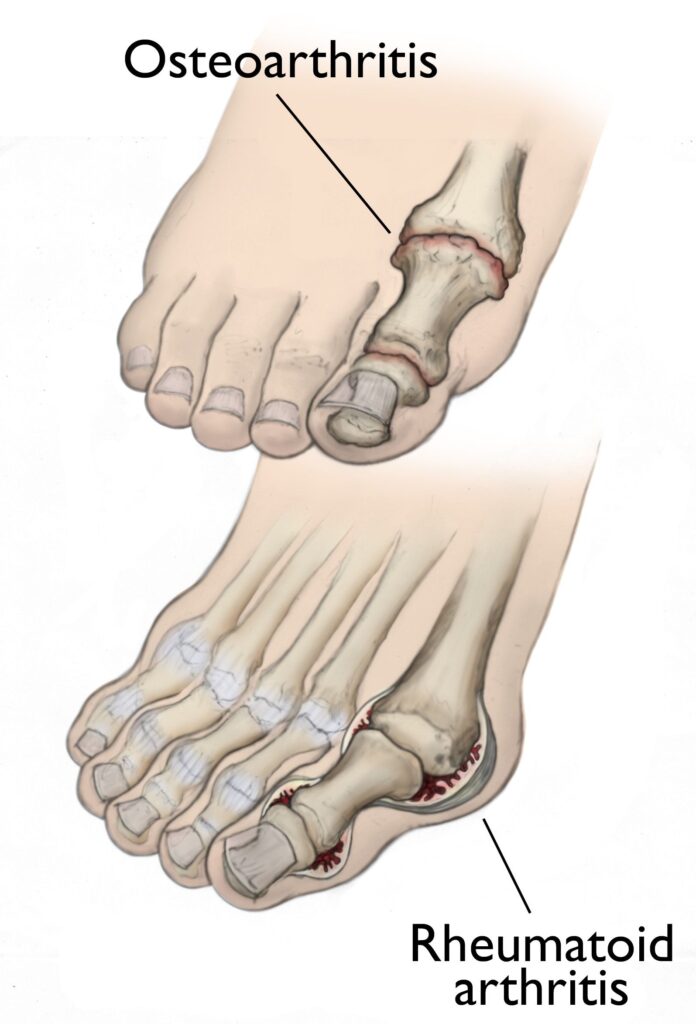
- Osteoarthritis: The most common form of arthritis, osteoarthritis is a degenerative disease that primarily affects weight-bearing joints like the hips, knees, and feet. It is caused by wear and tear on the joints, leading to thinning or destruction of cartilage. Factors like obesity, previous injuries, and genetic predisposition can accelerate its onset.
- Rheumatoid Arthritis: An autoimmune disease that causes inflammation in the synovial joints, including those in the hands and feet. It leads to pain, swelling, stiffness, and can also affect other organs in the body. Rheumatoid arthritis affects more women than men and typically appears between the ages of 25 and 50.
Management
While there is no cure for arthritis, symptoms can be managed effectively through a combination of treatments:
- Orthotic Devices and Footwear: Custom orthotics and specialized footwear can reduce the compressive forces on arthritic joints, improving mobility and reducing pain. The range of supportive footwear options has expanded, making it easier to find suitable shoes that accommodate different arthritic conditions.
- Exercise: Regular exercise is crucial for managing arthritis. It helps maintain muscle strength, stabilize joints, and reduce pain. Non-weight-bearing exercises, such as swimming or aqua jogging, are particularly beneficial as they minimize stress on the joints while keeping you active.
- Weight Management: Maintaining a healthy weight reduces the stress on arthritic joints, potentially slowing the progression of the disease.
- Surgery: In severe cases where conservative treatments fail, surgery to replace or fuse affected joints may be necessary. However, surgery does not always eliminate pain, so ongoing conservative care may still be required.
Foot arthritis can be a painful and limiting condition, but with appropriate management strategies, including the use of orthotics, supportive footwear, exercise, and weight management, many people can continue to lead active and fulfilling lives. If you suspect you have arthritis in your feet, get in touch and we can guide you through the best treatment options for your specific condition. For more general information take a look at Arthritis New Zealand website.



[…] There is evidence to suggest that there is a link to the early onset of osteoarthritis if joints are… […]