Can Posterior Tibial Tendon Dysfunction Be Cured?
- Experiencing pain on the inside of your ankle that's exacerbated by physical activity? - Struggling to stand up on the tiptoes of the affected foot because it feels too weak and painful? - Swear that your arches are appearing flatter? - Don't remember any notable injuries or sprains that could have caused your symptoms?
These are all red flags for a condition we see relatively often in podiatry called posterior tibial tendon dysfunction (PTTD). The name sounds intimidating - but it's actually a fairly straightforward condition to diagnose and treat, if you have the right knowledge, experience and tools like we have here at Waikato Podiatry.
Given that PTTD will affect almost one in ten people (8%) in some form, one of the most common questions that our podiatrists get around PTTD is whether it can be cured and be gone for good, today we're sharing everything you need to know about getting out of pain, living comfortably, and best settling yourself up to never have to deal with PTTD again.


Understanding Posterior Tibial Tendon Dysfunction (PTTD)
The best way to know how to fix a musculoskeletal pain or problem is understanding what it is, and why it has developed in your specific circumstances. So let's go over:
What is Posterior Tibial Tendon Dysfunction?
Down the back (and to the inside) of your leg, you have a tendon called the posterior tibial tendon, which then moves across to the inner ankle to connect to several areas on the bottom of your foot. The name "posterior tibial tendon" simply comes from the location of the tendon: the bulk of the tendon sits behind (posterior to) the tibia, which is larger of the two bones in the lower leg. The posterior tibial tendon plays an important role in the structure of our feet and the stability of our arches, and helps support healthy and pain-free movement every time you step, run, and maintain your balance during standing.
Causes of Posterior Tibial Tendon Dysfunction
PTTD is what we call an overuse condition, meaning that it is caused by repeditively overloading and straining the tendon past it's limits, leading to the onset of painful symptoms. Until the tendon has healed and regained full strength and function, it will not be able to effectively carry out its role. Contributing factors to the development of PTTD can include:
- Flat Feet - having a naturally flatter foot type can place more stress on the tendon with every step, maing it more vulnerable to injury
- Biomechanical or alignment issues in the feet, which can affect how the tendon is loaded
- Switching to flat, unsupportive footwear which can also overload the posterior tibial tendon, especially when it is used to being supported with better footwear.
- Past Injuries to the ankle or the posterior tibial tendon can weaken it, making it more susceptible to dsyfunction
- Walking or working on hard surfaces, which may increase the stress on the feet
- Regular physical activity such as running, long-distance walking, hiking and climbing stairs
- Increased bodyweight, which increases the demand on the tendon
- Conditions such as diabetes and hypertension
- PTTD is also more common in older women (compared to men), which is thought to be linked to a reduction in estrogen levels after menopause.

Symptoms And Stages Of PTTD
PTTD often affects one foot (typically the 'leading' or dominant foot, much like how you have a dominant hand), though it can develop in both feet. Without the right, evidence-based management, PTTD tends to progressively worsen - as do the symptoms. The end result can even be a partial tear, with a lengthier and more complicated recovery.
The symptoms you'll experience will depend on which stage of PTTD you're in (more of this below), but generally speaking, you may feel pain at the inner ankle, swelling or inflammation (including warmth and redness), and greater difficulty with movement involving the affected foot and ankle.
One important thing you should know is that PTTD is the most common cause of adult aquired flatfoot - one of the very few ways that arches can actually change and flatten in adulthood. This can make walking difficult as it alters your gait, increases the strain on other parts of the body, and can be a gateway to problems affecting the ankles, knees, hips and lower back. For reference, many sources use the terms 'PTTD' and 'adult aquired flatfoot' interchangeably.
If you're starting to recognise some of these symptoms, you should know that PTTD can be characterised into four stages of progression.
Stage one
Most people (and even some medical professionals who are less experienced with PTTD) tend to miss stage one because it comes with few symptoms - or even none that are really noticeable. Even if you're sent for medical imaging (like ultrasound), any significant abnormal findings, like tendon degeneration, will be absent. With this said, you may have some mild inflammation of the tissue surrounding the tendon that you or your podiatrist may identify, as well as some first-step pain in the mornings or after rest, which can be your first sign.
At stage one, you can also still perform this simple test called a single heel raise test:
- Hold onto the wall or a chair, beginning in a standing position and lift the unaffected foot off the ground.
- Attempt to lift onto the toes of the affected foot.
- At stage one, you should still be able to do this without any issues.
Stage Two
In stage two, the posterior tibial tendon shows damage that begins to interfere with it's normal function. Your foot might start to appear flatter, and medical imaging could you show the beginning of arch collapse. During a physical exam, you'll no longer be able to successfully perform the single-leg heel raise test.
Stage Three
Now we're getting into the more severe stages, with PTTD stage three being characterised by significant degeneration (breakdown) and deformities at the ankle. This causes significant movement restrictions. You'll experience significant pain at sinus tarsi - a small passageway at the ankle joint towards the outside of the ankle. Medical imaging will typically show ankle arthritis with an arch collapse.
Stage Four
By stage four, the deltoid ligament, which is located on the inside of the ankle and supports ankle joint stability, is compromised and there are degenerative changes at the ankle joint. The foot appears flat and rigid. You'll be experiencing ankle pain and severe sinus tarsi pain. As for imaging, it will show an arch collapse deformity, arthritic changes, and a tilt at a bone called the talus that forms part of the ankle.
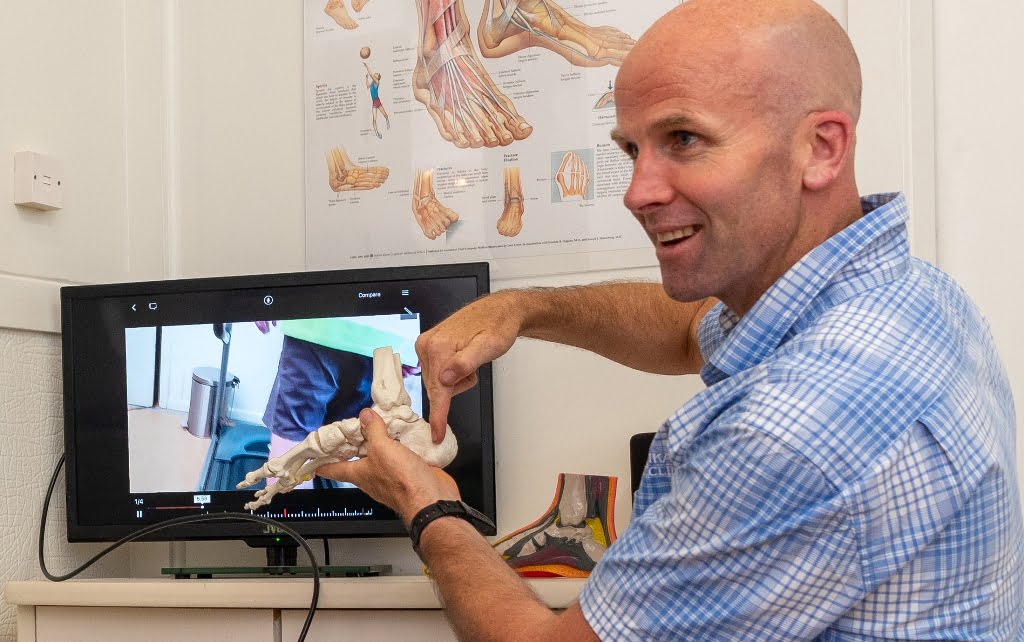
Diagnosing Posterior Tibial Tendon Dysfunction
Our Podiatrists here at Waikato Podiatry have the skills and experience to effictievely diagnose PTTD. Depending on your symptoms, we may also refer you for medical imaging to understand the bigger picture of your injury, especially if we suspect that multiple structures are damaged.
Treatment for Posterior Tibial Tendon Dysfunction
The earlier you can start managing PTTD and any related symptoms and causes, the better. This is as getting in early can go a long way in helping stop the progression of painful symptoms and further damage to the posterior tibial tendon.
When you first notice any symptoms, the PRICE principles (protection, rest, ice, compression and elevation) can be used to help reduce painful symptoms before you're able to see your podiatrist. Treatment then needs to focus on addressing the cause of PTTD in your specific case.
Our Podiatrists will discuss the range of treatment options with you, and depending on your circumstances and exam findings, this may include:
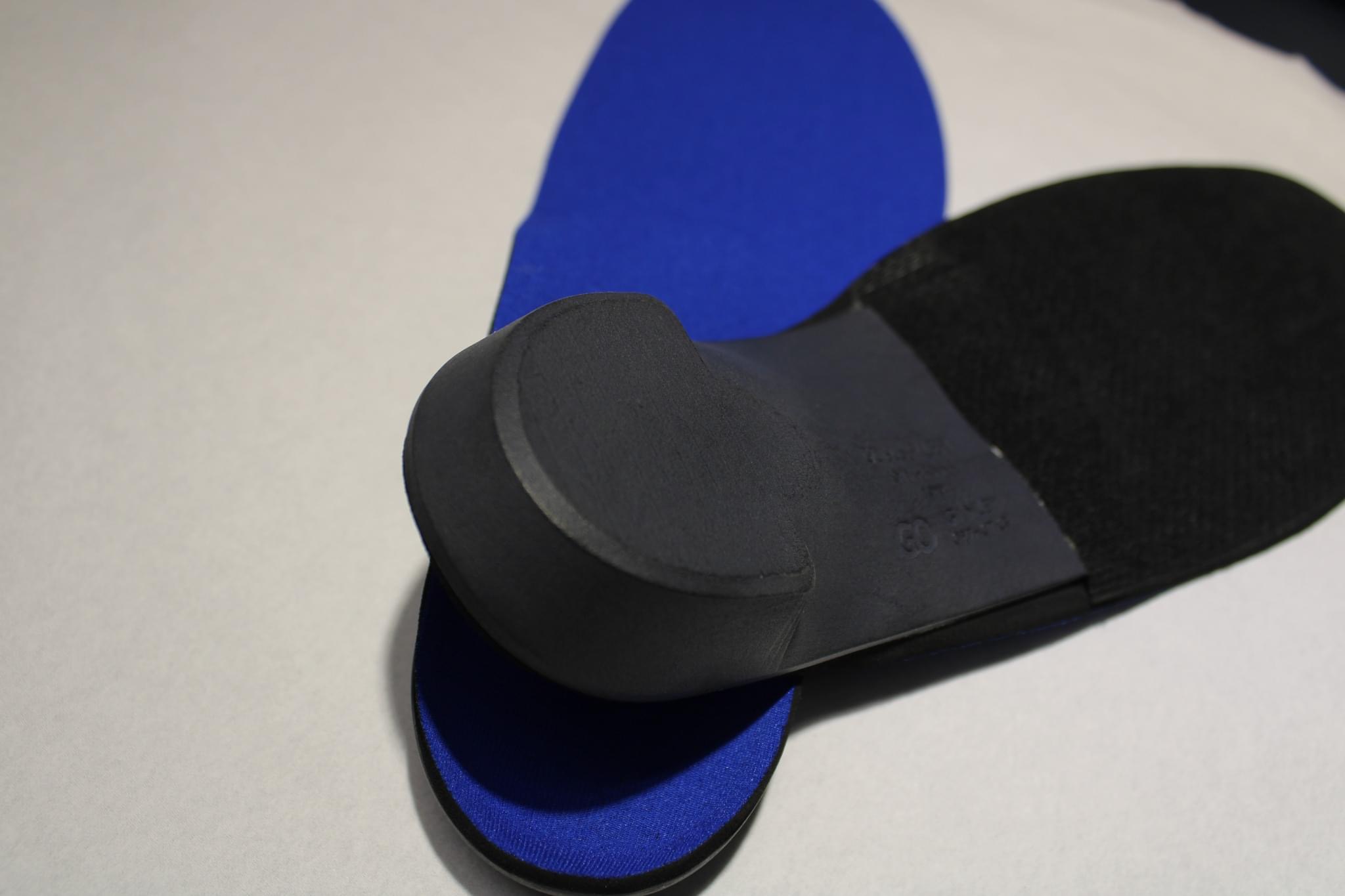
- Custom foot orthotics to support the posterior tibial tendon, support the arch, and correct any other biomechanical or alignment issues
- Supportive Footwear that stabilises the foot at the ankle and limits the foot rolling in and hence placing more strain on the posterior tibial tendon
- Stretching and Strengthening to address tight or weak supporting muscles
- Strapping the ankle to reduce strain on the tendon
- Activity Modification to reduce the strain on the posterior tibial tendon while it heals
- Where injury to the tendon is severe, such as a significant tear, a brace or cast may be required to completely off-load the tendon.
- If the PTTD is severe, a referral to explore surgical options may be necessary


Are Cortisone (Corticosteroid) Injections Useful For PTTD?
generally cortisone injections are not administered for this problem as it masks the pain and may reduce the strength of the tendon making it prone to further damage
Can Posterior Tibial Tendon Dysfunction Be Cured?
Posterior Tibial Dysfunction (PTTD) can be managed effectively, but whether it can be "cured" depends on the stage and severity of the condition when it is diagnosed. If you're currently in the early stages (stage one or two), then the conservative treatments we described are likely to successfully reduce your symptoms and improve your gait and foot function. In some cases, these treatments can restore the tendon's normal strength and function, effectively "curing" the condition, or at least preventing its progression. Evidence shows that early intervention with appropriate orthotics (meaning prescription from your podiatrist, instead of one-size-fits-all orthotics) and physical therapy can lead to significant improvements.
For the more advanced stages (stages three and four), where there is significant tendo degeneration and deformity, conservative treatments may not be sufficient to offer a "cure" - though they can still be helpful in reducing pain and improving comfort. In these cases, surgical intervention is often required to correct the deformity and restore function. Procedures can include tendon repair or transfer, osteotomies (bone cuts), and in severe cases, joint fusion. While surgery can significantly improve symptoms and functions, it is more about managing the condition rather than providing a complete cure.
Can PTTD Go Away on Its Own?
PTTD generally does not resolve on its own. Without treatment, it tends to worsen over time, leading to increased pain and further deformity. This is where early intervention with the help of your podiatrist can help manage symptoms and prevent progression, but simply ignoring the condition typically results in worsening symptoms.
How Long Does It Take to Recover from PTTD
The recovery time for PTTD varies depending on the severity of the condition and the type of treatment. For mild to moderate cases (stages one and two), it can take several months of consistent use of orthotics, physical therapy, and other conservative treatments to see significant improvement. For more severe cases (stages three and four) that require surgical intervention or other severe measures, recovery can take six months to a year, including a period of immobilisation followed by rehabilitation.
What Activities Should Be Avoided with PTTD?
With PTTD, it's important to avoid activities that put excessive strain on the posterior tibial tendon. This includes high-impact activities such as running, jumping, and heavy lifting. Prolonged walking, especially on hard surfaces, and standing for long periods should also be minimised where possible. Low-impact activities like swimming or cycling can be good alternatives that allow you to stay active without exacurbating the condition. Your Podiatrist will be able to give you advice on this specific to your circumstances.
To book an appointment with our podiatry team here at Waikato Podiatry, call us on 07 838 0003, or use our online booking portal.

Thank you for such valuable information.